Cancer is a disease caused by abnormal cell growth. The cells’ genetic material is corrupted and the metabolic processes do not interact well with them anymore. They grow unchecked, mostly in the form of a lump. The immune system does not necessarily recognise the danger of the cells in the tumour or have the right tools to fight it.
A promising field hopes to change that: immunotherapy could stimulate the body to kill the cancerous cells by itself. Sadly, for now, immunotherapy only works on a few select cancer types such as kidney cancer, bladder cancer or Hodgkin’s lymphoma.
But researchers at the Massachusetts Institute of Technology (MIT) have recently made a breakthrough on that front. They have found a way to “reawaken” the immune system to the tumour’s threat. This new method could open up more types of cancer to be treated by immunotherapy.
How the immune system reacts to cancer
Fevers, aches and pains, inflammation and swelling are often symptoms indicating that the immune system is actively fighting threats, but its effect can be less noticeable yet much more impactful : it has been found that some immune cells help clear out dead brain cells after a stroke and that some other immune cells help the heart maintain a steady beat.
Cancers usually develop forms of defence against the host’s immune system. So, while the immune system’s primary function is to identify and fend off threats like native and non-native mutated cells posing a threat to the system, tumours have developed ways to circumvent it altogether, and sometimes, they even make it work against us.
Strength of the immune system…
Our immune systems are a refined and precise line of defence. But cancer is a powerful disease: when cancer grows unchecked, it is because it has simply overpowered the immune system. As a matter of fact, simply put, if we did not have immune systems, we would all have cancer.
The immune system is constantly battling out cancerous cells “in the background” while we go about our daily lives. Over time, whether because cancerous cells have grown in strength and number or because our immune systems are weakening, tumours may grow unchecked. Scientists are still not sure what causes that “tipping point” from “background threat” to “overpowering major health risk”, there may not even be a clear separation line for all we know.
It also depends on the cancer, sometimes the tumour’s DNA is responsible for the situation, sometimes it is the very cancerous cells’ aggressiveness. Even worse, some cancer cells have been shown to mislead immune cells into helping cancer grow and expand throughout the body. For instance, some immature immune cells have been “deceived” by cancer cells into not growing to a stage at which they could recognize and fight it.
… A story of balance
To get a clearer picture, it can help if you conceive of the immune system as being in a constant state of balance: when it is balanced, it should kill tumours; however, any perceptible enough imbalance may provide the environment for tumours to grow into a dangerous metastatic disease.
More specifically, in the case of breast cancer, cells from the immune system (namely macrophages, which fight off “intruders” by “digesting” harmful matter) can be “recruited” early in their life cycle by the tumour.
They then become “tumour-associated macrophages” (or TAMs), which will not only miss their ability to digest tumour cells, but also prevent them from being killed and help them spread to other tissues and organs.
Researchers captured the whole process on film in lab mice, in which we can see breast cancer cells and macrophages “work together” to help cancer spread through the bloodstream.
The immune system, a double-edged sword
However, while examples like TAMs can be grim, recent research has hypothesised that immunotherapy drugs could target these “rogue” immune cells as well as older ones to kickstart the immune system into attacking tumours again with renewed vigour.
A novel compound called TMP195 is designed to reactivate TAMs for their original purpose. Research has been conclusive on breast cancer in mice. In the same vein, MIT researchers have found a way to restart the immune system’s normal functioning by removing tumour cells from the patient’s body, treating them with chemotherapy drugs, and then injecting them back into the tumour.
The process is simple: before injecting them back, doctors administer drugs that stimulate the immune system’s T cells (there are two types: helpers that stimulate B cells to make antibodies; and killers that directly attack cells); after injection, the immune system properly recognises the tumour as a threat thanks to the combined action of the drugs and the treated tumour cells.
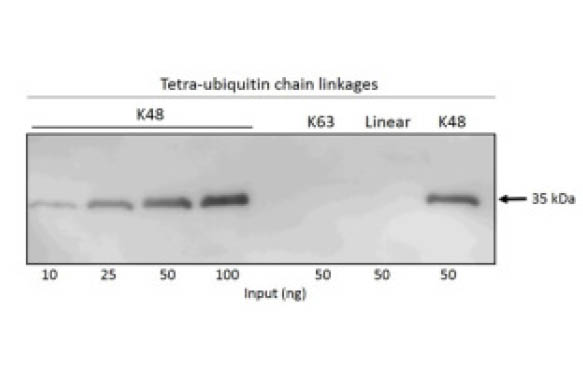
Again, laboratory testing on mice was conclusive: tumours were completely erased from about half the mice’s bodies. The scientists understood the mechanism that prompted the immune system back into action: tumour cells that were damaged by the chemotherapy drugs but were still alive spurred it back into action way better than if they had died.
The reason for this is the DNA damage caused by the drugs: the stress of this damage sent signals that galvanised T cells which then not only destroyed the damaged cells but also the “healthy” tumour cells.
Successful tests
Not only did this new treatment prove very efficient in the short term on melanoma and breast tumours in mice, but continued observation also showed that the mice’s immune systems reacted to the injection of new tumour cells several months later and destroyed any injected cells before they could even form a tumour.
Unlike chemotherapy and radiation therapy, immunotherapy drugs do not directly kill cancer cells, they instead aim to use the powerful weapon humans already have at their disposal: the immune system. Immunotherapy is a way to inform the body of the threats it has stopped combating.
In the long run, it may even help patients heal from tumours on their own, without severely damaging their health with invasive surgery and toxic drugs. It is a very promising field with a bright future, but further testing is required to fully understand the mechanics at work and all their potential (positive and negative) effects on patients.