A symposium on trends in Clinical Oncology was recently held in Madrid, Spain. The symposium gathered actors from the private health system (Hospital Madrid – Clara Campal, Onkologikoa, Clínica Universidad de Navarra), as well as pharmaceutical companies (Roche, Novartis).
The interest of this symposium is that it had a look at the research on cancer from the perspective of clinicians coming from private hospitals, and not from the National Health Systems.
In Europe, cancer research and clinical studies are mainly performed in organisms belonging to the Government. Still, research and clinical practice in private entities is growing, not only in assistential terms, but also for translational research and clinical studies, especially Phase I and IIa / IIb.
All speakers agreed that personalised medicine is a growing trend in Oncology, and moreover, it is absolutely mandatory to integrate the latest developments in Oncology in daily practice, meaning that MDs should keep up to date with all research involving diagnostic and prognostic biomarkers. The concept of predictive medicine was also mentioned several times.
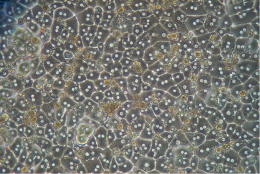
Many of the current biomarkers for cancer rely on SNPs and are based on DNA sequence. However, role of other biomarkers (e.g. secretome, miRNAome, imaging) is increasing. This will lead to an increase in the precision of the diagnosis, as well as adjusting the treatments to the different phases of the disease. Cancer is a group of different diseases, and they evolve in time, so the treatment that works for one patient does not work for another, and even the treatment that worked in the past for one patient may not work in the future. A continuous assessment of biomarkers is needed in order to optimise the treatments.
Cancer research involves at least 30 % of the resources of pharmaceutical companies in Europe. In Spain only, there are currently 744 cancer-related clinical studies being performed (294 of these in private hospitals). For these clinical studies, biologics are growing as a novel therapy with higher efficiency and more stringent cohort definitions (i.e. characterisation of responding populations) to allow them to enter into reimbursement programs.
Trends in clinical assays aim at including biomarkers in very early phases, and joining Phases I and II into a mixed phase (I-II). Patients enrolled in clinical assays are now characterised, before treatment, for their molecular profile, in order to know and predict, a priori, any possible adverse effects of the therapy (or elucidate causes of non-responsiveness). This will mean that number of patients will be lower in future clinical assays, and a network will be key in order to achieve a significant number of patients, as a few hospitals may not have all the patients needed in a clinical study.
At the Biomarkers team at tebu-bio, we are glad to assist some of this translational & clinical researchers all over Europe to help them win the battle against cancer.



2 responses
Very interesting information here. I wonder if these biomarkers will begin emerging in treatments for diseases other than cancer. Cancer, much like influenza, is constantly evolving and will vary between patients, so it is important that the treatments for cancer are adaptable to each person.
Thanks for your comment, Matthew. Biomarkers are emerging everywhere, but it is also true that Oncology is the leading disease. Indeed, the notion of personalised medicine aims at developing treatments (or a combination of treatments) specific for each health state, that can vary between persons…and also in the same person over time.
A different story, though, may be whether these personalised treatments and the tests they require will be affordable by each and every patient. In any case, research on biomarkers is also associated to developing tests that have the lowest possible cost.